(BROOKLYN, Ny.) For more than 30 years Marline Mclean has fought an uphill battle against diabetes, from changing daily habits, to monitoring blood levels and struggling with the drug costs, including insulin.
Calling Flatbush home for more than 45 years, Mclean takes pride in the vibrant community. Her Jamaican roots influence everything from her cooking to her deep sense of resilience.
“When I was first diagnosed, I was in denial,” she says. “I knew the numbers said I had it, but I didn’t change my eating habits.” For years she has relied solely on Metformin without making the lifestyle changes needed to manage her condition effectively.
Now 69, McLean spent much of her career as a hematology technologist, prioritizing her work and caring for others above her own well-being. It wasn’t until her retirement at 62 that she finally took control of her health. A pivotal moment came when she started using a continuous glucose monitor, a tool she initially resisted. To her surprise, the monitor revealed how even her morning coffee with creamer spiked her blood sugar by 40 points. Now she manages her diabetes with insulin, Metformin and careful food choices.
Despite these challenges, she finds joy in activities like swimming at her local recreation center and taking online classes, ranging from French and Italian to Python coding and yoga, saying they keep her mind sharp and her spirit grounded.
Brooklyn is home to one of the largest concentrations of people with chronic health conditions in neighborhoods such as Bedford-Stuyvesant, East New York, Brownsville. In these predominantly Black and Hispanic communities diabetes rates are disproportionately high with 10.5% of residents living with the disease.
Mclean’s story reflects a larger crisis in Brooklyn. She considers herself fortunate that her costs are covered by Medicare unlike hundreds of other Brooklyn residents who are uninsured or rely on private plans. She doesn’t have to make impossible choices between health and necessities. However, uncertainty looms as many others wonder, “What now?” under a second Donald Trump presidency, with fears that the President Joe Biden-era measure capping insulin costs at $35 could be suspended.
And, gaps in coverage remain despite recent New York legislation to eliminate insulin cost-sharing for those on state-regulated health insurance plans including Medicaid, Medicare, and marketplace policies. Many underinsured individuals, particularly those with self-funded employer health plans, continue to struggle with the cost of insulin. About 8% of the borough’s adult population lack health insurance coverage, compared to 10% nationwide.
Before the Biden plan cap of $35, the average out-of-pocket cost for insulin prescription in 2019 was $58, with those on private insurance or Medicare paying an average of $63 per monthly fill. For many Brooklyn families, the financial burden forces choices between purchasing life-sustaining medication and basic needs like rent or groceries.
“Sometimes it’s a choice between buying insulin and paying rent,” said Janine Allen, a diabetes health coach at One Brooklyn Health, a network of healthcare providers serving neighborhoods in East and Central Brooklyn, including Carnesie and Prospects Lefferts Gardens.
In the heart of Bedford-Stuyvesant, Pierre Toussaint Health Clinic sits on a bustling street, surrounded by bodegas, family-owned businesses, and long-standing cultural institutions that reflect the neighborhood’s history. Allen sees firsthand the devastating impact of unaffordable medications on her patients, many of whom also struggle to afford other diabetes treatments like Metformin, Januvia, and GLP-1 drugs — medications essential for preventing complications. “One patient told me their blood sugar levels went up, not because they weren’t trying, but because they simply couldn’t afford their medications,” she said.

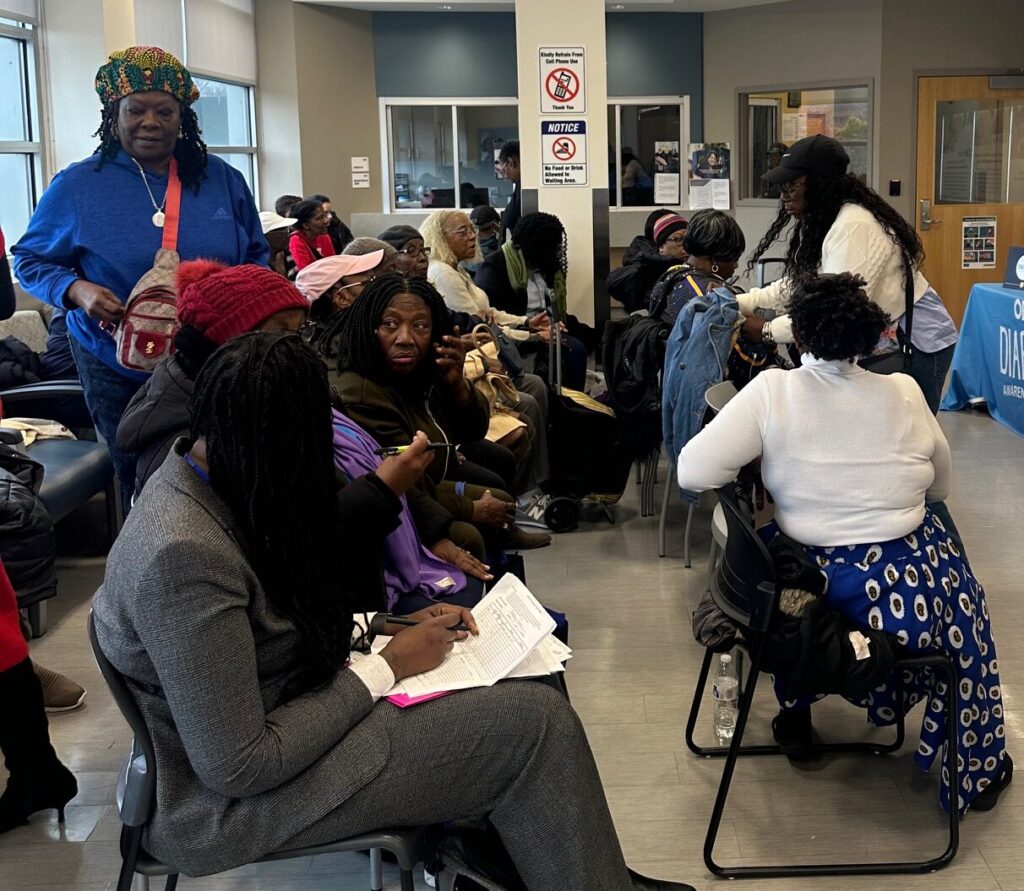
Photo credit: Pierre Toussaint Family Health Center
In mid-November the clinic’s annual World Diabetes Day gathering brought more than 50 residents, health professionals and advocates to discuss medication access, share early detection strategies, and explore practical solutions for thriving with diabetes. Attendees also connected with representatives from an insulin pump company, whose affordability program makes it more accessible to those struggling with costs.
Lapses in insurance coverage often lead to life-threatening complications. “If someone couldn’t get insulin, there could be a great impact on their health,” said Dr. Kurt Kodroff, an endocrinologist at One Brooklyn Health.
The clinic takes a team-based approach to diabetes care, focusing on healthy eating, exercise, stress management, and sleep hygiene. “We treat the whole person, not just their diabetes,” he said, referring to the team of certified diabetes educators, health coaches, dietitians, nurses, and social workers.

Chef Yusef Webb at OBH Diabetes Day in Brooklyn, NY. ( Photo: Valerie Agyeman)
Building on this holistic perspective, a local chef, Yusef Webb led a cooking lesson, showing diabetics how to create simple meals with ingredients to stabilize their blood sugar. The demonstration introduced nutrient-rich foods such as chickpeas, leafy greens, tomatoes and low-sugar dressings. Residents eagerly participated by tasting samples and collecting recipe cards to take with them to try at home. “It’s not just about medication, it’s about understanding how food impacts your body which is critical in managing diabetes,” Webb said.
As Mclean sat among her friends savoring a plate of vegan desserts and an array of fruits, it was a reminder of how far she has come in her journey. Reflecting on the challenges faced by many, she said, “No one should have to choose between their health and basic needs.”